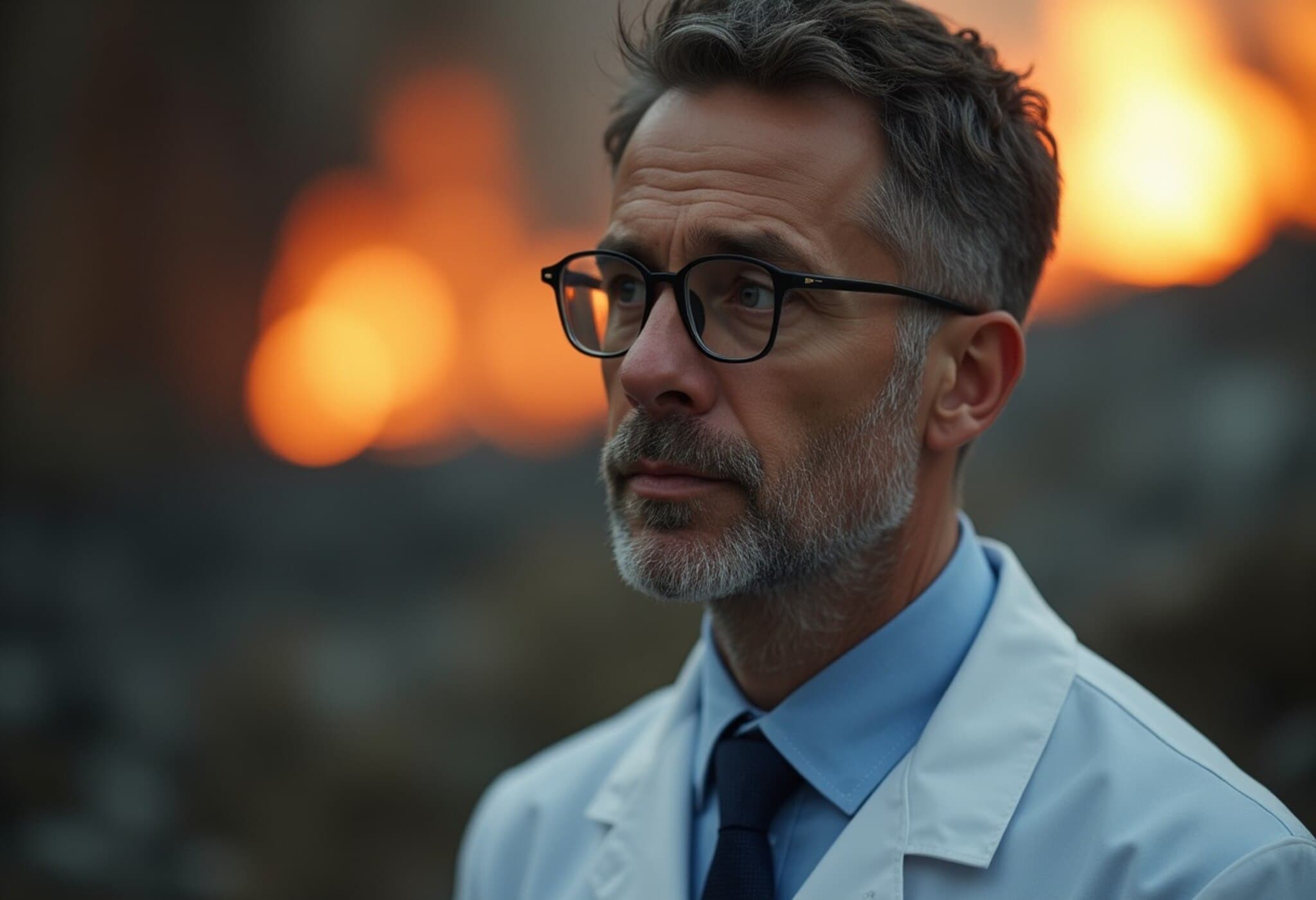
German Doctor Faces Trial Over 15 Patient Murders and Arson Charges
In a chilling case that has gripped Germany, a 40-year-old physician, known only as Johannes M. under strict German privacy protections, stood trial in a Berlin regional courtroom beginning July 14, 2025, accused of murdering 15 palliative care patients and setting their homes ablaze in attempts to cover his crimes.
Charges and Legal Stakes
The prosecutor's office alleges that Johannes M. committed premeditated murders driven by “base motives”, charging him with 15 counts. Authorities are seeking a life sentence without parole eligibility for at least 15 years, a particularly stringent measure reserved for especially grave offenses under German law. In addition, he faces a permanent ban from practicing medicine and preventive detention to guard public safety.
Alleged Crimes and Modus Operandi
Johannes M. served as part of a nursing service specializing in end-of-life care. Prosecutors claim that between September 2021 and July 2024, he administered lethal doses of anesthetics and muscle relaxants to vulnerable patients aged between 25 and 94. These drugs were given without the patients’ consent and led to rapid respiratory failure and death in most cases, often occurring in their own homes.
Investigators suspect that to mask the killings, Johannes M. attempted to destroy evidence by setting fire to victims’ residences. These heinous acts have cast a stark spotlight on patient safety protocols in Germany’s palliative care system.
A Disturbing Case Example
One particularly harrowing case involves a 56-year-old woman who died in September 2021. According to court documents, the doctor administered lethal medication without medical necessity, then falsely summoned emergency services under the pretense of a critical event. When paramedics revived the woman and transported her to hospital, Johannes M. reportedly contacted her family, admitting to violating the patient’s living will prohibiting life-prolonging measures. With the daughter’s consent, medical staff ceased artificial respiration, leading to her death days later.
The Elusive Motive and Mental Health Questions
Despite the severity of the allegations, the doctor has so far refused a pre-trial psychiatric evaluation. The court has decided an expert witness will examine his mental state during proceedings. Johannes M.’s attorney, Christoph Stoll, has declined to comment on the case at this stage. Notably, many of the victims were chronically ill but not in immediate danger of dying, raising unsettling questions about the motives behind the killings.
Scope of the Investigation and Wider Implications
The trial is slated for an extensive run, with 35 sessions scheduled until January 2026. It features 13 relatives as co-plaintiffs and up to 150 witnesses, underlining the complexity and emotional weight of the proceedings. The investigation has expanded significantly; a specialized homicide unit has already reviewed 395 related cases, confirming suspicions in 95 instances and investigating 75 others. Among the ongoing inquiries is the suspicious death of the doctor’s cancer-stricken mother-in-law.
Authorities plan to exhume five bodies for further forensic examination. This case echoes the notorious 2019 conviction of a German nurse sentenced to life imprisonment for the murder of 87 patients, highlighting systemic vulnerabilities in healthcare oversight.
Expert Analysis: Challenges in Policing End-of-Life Care
This case shines a harsh light on the delicate balance between compassionate palliative care and safeguarding vulnerable patients from abuse. Experts emphasize the urgent need for rigorous monitoring within home-care services, robust ethical training, and transparent reporting mechanisms to reduce risks of malpractice and criminal acts masked as medical intervention.
Furthermore, Germany’s legal framework faces a test in addressing euthanasia-related crimes, distinguishing lawful end-of-life choices from criminal acts driven by malicious intent. The inability or refusal to assess a defendant’s mental health in such cases adds further complexity to both prosecution and defense strategies.
Critical Questions Raised
- How can medical systems improve oversight without compromising patient dignity and autonomy?
- What safeguards must be enhanced to prevent similar tragedies in home-care settings?
- How should courts handle defendants who refuse psychiatric evaluation, especially in cases involving life and death?
- What lessons can policymakers learn to tension the delicate ethics surrounding end-of-life care?
Editor’s Note
This ongoing trial underscores profound challenges in healthcare ethics, law enforcement, and patient rights. While the German courts rigorously pursue justice, the human toll on survivors, families, and healthcare providers resonates deeply. As investigations continue, this case serves as a sobering prompt for policymakers worldwide to fortify protections around vulnerable patients and reflect on the moral complexities inherent in end-of-life care. Readers are encouraged to watch how this legal saga unfolds and consider the broader implications for medical accountability and trust.